Healthcare Professionals Seek Social Connections When Moving to Rural Towns
- by John Pender
- 5/8/2023
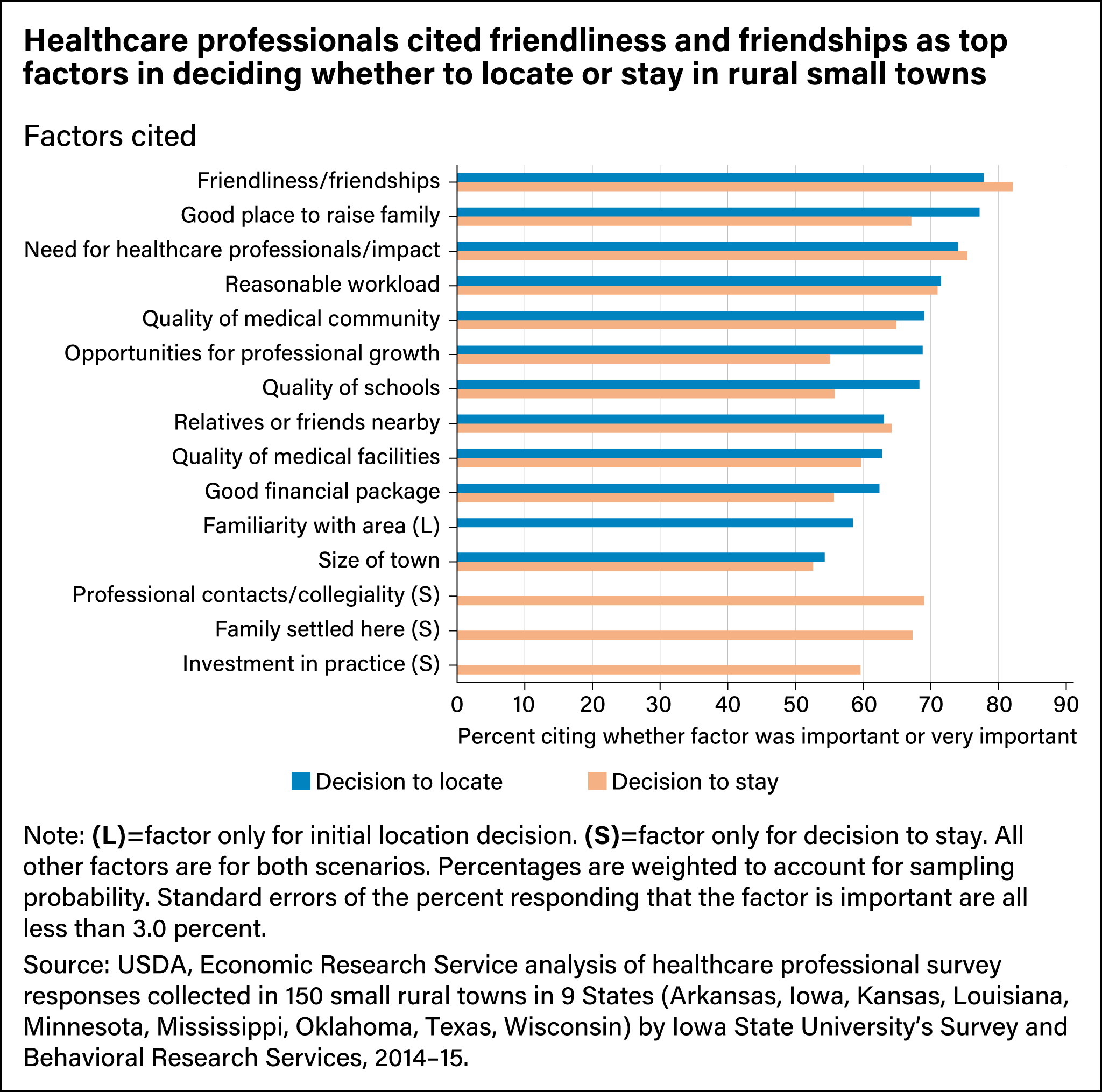
When choosing rural locations in which to practice, healthcare professionals most often cite social factors such as the friendliness of the town, according to a survey administered by researchers at USDA, Economic Research Service and Iowa State University. Similar factors come into play when they decide to stay in their rural small towns, the survey showed. More than 900 physicians, nurse practitioners, physician assistants, certified nurse midwives, and dentists responded to the survey, conducted in 2014 and 2015. They lived in 150 rural small towns in Arkansas, Iowa, Kansas, Louisiana, Minnesota, Mississippi, Oklahoma, Texas, and Wisconsin. For rural communities to attract and retain healthcare professionals, researchers found that factors in decisions to locate and stay in rural small towns usually included the following: personal and professional relationships (known as social capital), people-related resources such as education, skills, and health (human capital), and physical capital such as the town’s infrastructure and medical facilities.
Among social capital-related factors, healthcare professionals most often cited friendliness as an important factor in their decision to locate in the study towns, and they put friendships with local people at the top of their list of reasons to stay. Other factors that reflect the importance of social relationships included having relatives or friends living nearby, if the professional’s family was settled in the town, the quality of professional contacts and collegiality among local healthcare professionals (investigated only for the decision to stay) and being familiar with the area (for the initial location decision).
Human capital-related factors, such as the quality of the medical community, the quality of schools, and opportunities for professional growth were often cited as important. The availability and quality of some types of physical capital—such as medical facilities and schools—mattered to most healthcare professionals as well.
Some factors desired by most healthcare professionals reflect a combination of social and other components. For example, being a good place to raise a family often was indicated as important in both initial location choice and in the decision to stay. Responses to open-ended questions suggest that being a good place to raise a family was associated with social opportunities and relationships, safety, the quality of local schools and infrastructure, natural amenities, and other characteristics related to multiple types of community assets. Many healthcare professionals discussed the advantages of small-town life in similar terms, especially the benefits (and drawbacks, such as lack of privacy) of personally knowing their patients and many others in the town.
Besides factors that could be described as a community capital, one of the most cited points in both location and retention decisions was the need for healthcare professionals in the community. Other characteristics of the medical/dental practice or job, such as workload and the quality of the financial package offered, also were cited as important. One factor that was particularly important for dentists in deciding to stay was the investment they had made in their practice. The survey showed dentists were much more likely than other healthcare professionals to own their practice.
Some factors were cited as important by less than half of healthcare professionals (in decreasing order of how often cited): natural amenities, recreational opportunities, career opportunities for a spouse or partner, availability of goods and services, social opportunities, the opportunity to own a medical or dental practice, low cost of living, recruitment or retention efforts by the community, low taxes, cultural amenities, and placement by a Government program.
This article is drawn from:
- Pender, J., Kuhns, M., Yu, C., Larson, J. & Huck, S. (2023). Linkages Between Rural Community Capitals and Healthcare Provision: A Survey of Small Rural Towns in Three U.S. Regions. U.S. Department of Agriculture, Economic Research Service. EIB-251.
You may also like:
- Dobis, E.A. & Todd, J.E. (2022, July 5). Self-Employed Workers Are Less Likely To Have Health Insurance Than Those Employed by Private Firms, Governments. Amber Waves, U.S. Department of Agriculture, Economic Research Service.
- Dobis, E.A. & McGranahan, D. (2021, February 1). Rural Residents Appear to be More Vulnerable to Serious Infection or Death From Coronavirus COVID-19. Amber Waves, U.S. Department of Agriculture, Economic Research Service.
- Dobis, E.A. & Todd, J.E. (2022, August 1). The Most Rural Counties Have the Fewest Health Care Services Available. Amber Waves, U.S. Department of Agriculture, Economic Research Service.
- McGranahan, D. & Parker, T. (2021). The Opioid Epidemic: A Geography in Two Phases. U.S. Department of Agriculture, Economic Research Service. ERR-287.
We’d welcome your feedback!
Would you be willing to answer a few quick questions about your experience?