Households With at Least One Obese Child Differ in Several Ways From Those Without
- by Young Jo
- 12/4/2017
The prevalence of childhood obesity in the United States has more than tripled since the 1970s. According to statistics from the U.S. Centers for Disease Control and Prevention (CDC), about 1 out of 5 children and adolescents (ages 2-19) were obese in 2011-14. (An obese child/adolescent is one whose body mass index (BMI) is at or above the 95th percentile of the sex-specific CDC BMI-for-age growth chart.)
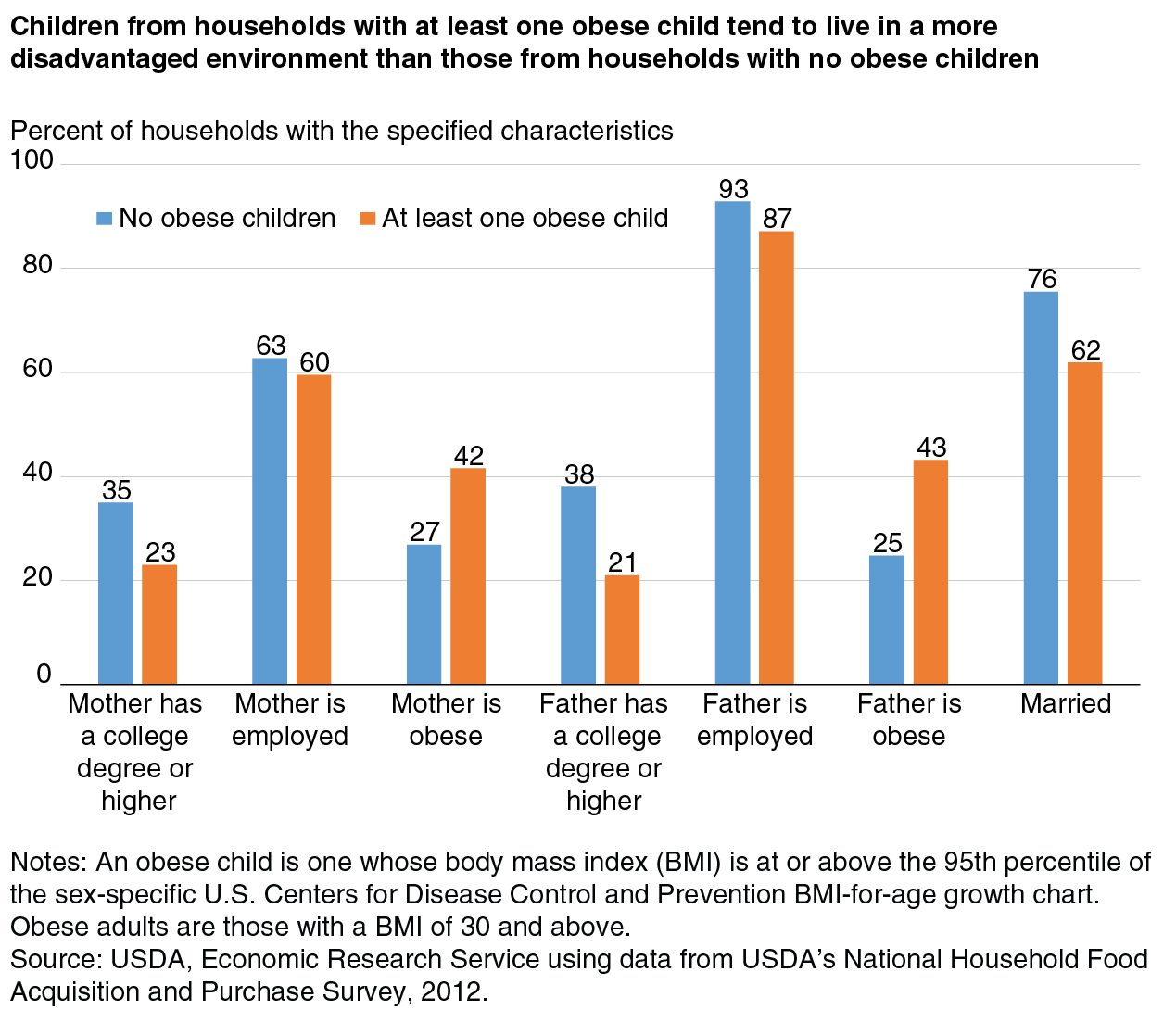
To better understand childhood obesity, ERS researchers examined how households with at least one obese child (obese-child households) differ from those without obese children (nonobese-child households). Using USDA’s National Household Food Acquisition and Purchase Survey (FoodAPS), the researchers found that children from obese-child households tend to live in a more disadvantaged environment compared with children from nonobese-child households. Their parents were more likely to be unmarried, less educated, unemployed, and obese themselves. For example, less than a quarter of mothers (23 percent) and fathers (21 percent) had a college degree or higher among obese-child households compared to over a third of mothers (35 percent) and fathers (38 percent) among nonobese-child households. Also, the shares of obese fathers and mothers were almost twice as large among obese-child households as the shares among nonobese-child households.
Analysis of FoodAPS data revealed that children from obese-child households also had slightly lower access to healthful foods. In rural areas, obese-child households were more likely to reside in areas with less availability of superstores and supermarkets, where fresh produce and other healthful foods are readily available. For example, obese-child households in rural areas had one less supermarket within a 10-mile radius of their residence compared to nonobese-child households.
In urban areas, obese-child households were more likely to reside in areas with greater availability of convenience stores, where high-calorie snack foods make up most of the food offerings. Obese-child households in urban areas had one more convenience store within a 1-mile radius of their residence compared to nonobese-child households. These findings highlight potential characteristics that may be helpful in identifying groups of children at higher risk of obesity.
This article is drawn from:
- Jo, Y. (2017). The Differences in Characteristics Among Households With and Without Obese Children: Findings From USDA’s FoodAPS. U.S. Department of Agriculture, Economic Research Service. EIB-179.
We’d welcome your feedback!
Would you be willing to answer a few quick questions about your experience?