Federal Support for Nutrition Research Trends Upward as USDA Share Declines
- by Fred Kuchler and Andrew A. Toole
- 6/1/2015
Highlights
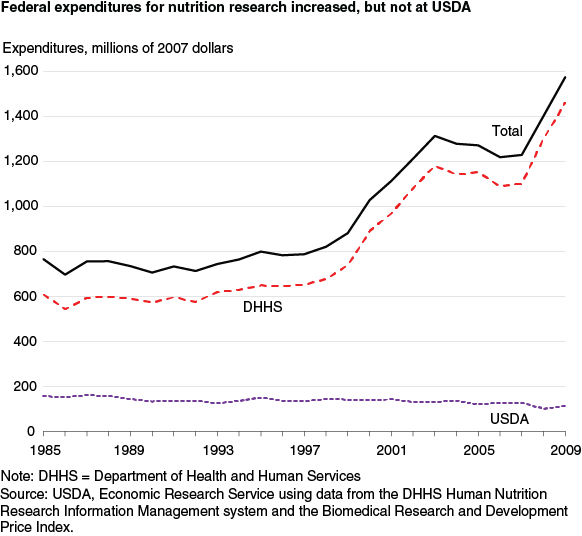
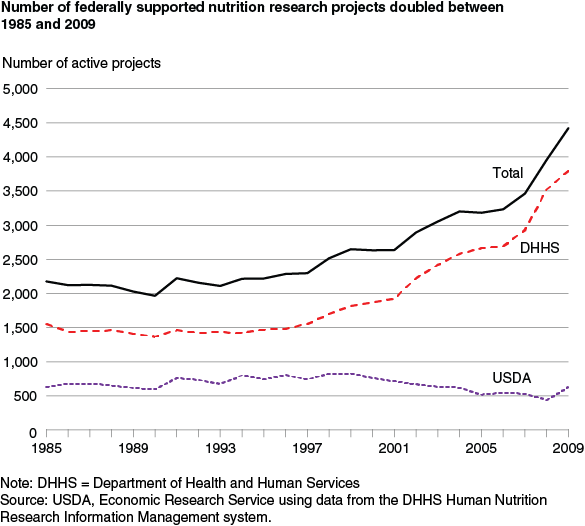
- ERS research shows that Federal investments in nutrition research more than doubled in real terms from 1985-2009.
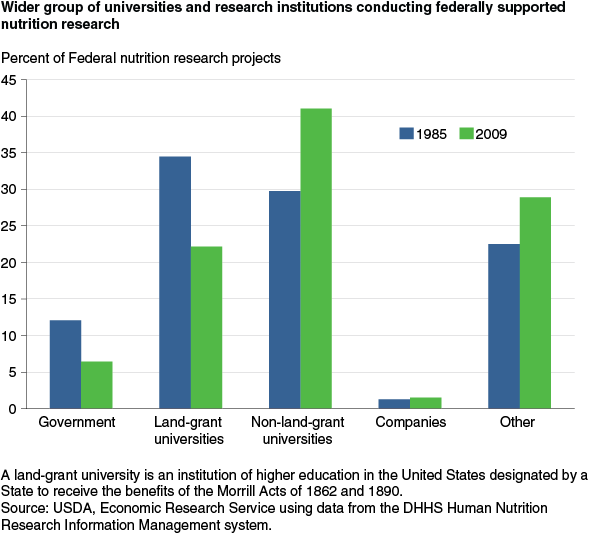
- The share of Federal funding by the U.S. Department of Health and Human Services increased while USDA's decreased, with a broader set of academic institutions conducting nutrition research in recent years.
- Over this period, increasing support has been directed toward addressing chronic conditions and diseases while interest in food science has waned.
Nutrition research plays a key role in the health and well-being of a country’s citizenry. From fortifying commonly consumed foods with essential vitamins and minerals to providing the scientific underpinnings for Federal food regulations, human nutrition and health research has garnered many successes for the U.S. public health community. In its early days, nutrition research established linkages between dietary deficiencies and afflictions and identified the structures of vitamins, thus allowing vitamins to be synthesized on an industrial scale.
More recently, nutrition research has been the basis for Federal regulations on food label claims and the standards for meals and snacks sold in schools. Nutrition research also underlies the Dietary Guidelines for Americans—a joint effort of the U.S. Department of Health and Human Services (DHHS) and USDA to provide the Nation with recommendations for a nutritionally balanced diet. The Guidelines are the foundation for Federal nutrition education materials, and they influence the level and type of food assistance offered through USDA’s 15 food and nutrition assistance programs.
A recent ERS analysis of data maintained by DHHS’s National Institutes of Health (NIH) shows that Federal investments in nutrition research more than doubled in real (inflation-adjusted) terms from 1985 to 2009 due to increased DHHS funding, especially between 1999 and 2003. Along with this growth in funding, the portfolio of nutrition research—the types of studies and who conducts the research—has changed, with implications for the nutrition-related health problems that might be addressed and solved, the guidance consumers receive on choosing a healthy diet, and the type of Federal intervention that occurs in consumers’ food choices.
Early—and Later—Food Fortification Successes
In the early part of the twentieth century, micronutrient deficiency was a common problem for Americans. Iodine deficiency can cause the thyroid gland to enlarge—goiter—and until the early 1920s was endemic. Niacin deficiency—pellagra—had emerged as a major killer. Rickets, scurvy, and beriberi were common—all caused by dietary deficiencies. The solution that virtually eradicated these problems was food fortification, adding micronutrients to commonly consumed foods. Iodine was added to salt, B vitamins and iron were added to flour, and vitamin D was added to milk.
However, finding a way to augment Americans’ intake of vitamins proved contentious. For each identified dietary deficiency, the young science of nutrition research was required to demonstrate the benefits that were likely from fortification. The questions that salt manufacturers asked about iodized salt are nearly identical to questions that are now asked about proposed food regulations (see box, “Public Health Regulations Rely on Nutrition Research”).
More recently, the U.S. Centers for Disease Control and Prevention credited regulations requiring folic acid fortification of grain products as reducing neural tube birth defects by about a third. In this case too, food fortification proved to reduce a serious health problem and did so without interfering with consumers’ food habits.
Doubling of NIH’s Budget Boosted Nutrition Research
It ought not to be surprising that the Federal Government is a large supporter of U.S. nutrition research. When nutrition research is successful, it produces new knowledge and information, a commodity that is often difficult to market. For example, suppose a food manufacturer considers conducting research on whether a serious health problem can be solved with a minor recipe change. The manufacturer’s financial incentive to conduct that research would be the promise of marketing a product to consumers who would pay a premium for a food that solves a health problem. However, this price premium is not likely to last long. A manufacturer cannot inform consumers about the new product and the associated health benefits, while keeping competitors from finding out. Competitors would likely offer the same product without incurring the expense of research, and competition would drive prices back to where they started. The manufacturer has little incentive to conduct the research. Instead, the public sector might have to step in.
DHHS’s NIH maintains a database on Federal support for nutrition research called the Human Nutrition Research Information Management (HNRIM) system. Since 1985, when the HNRIM database became operational, participating agencies provided data on active nutrition projects each year. USDA’s contribution ended with 2009 data. Most of the information provided came from DHHS and USDA. Over time, new projects were entered into the database, and completed projects were no longer reported.
Federal financial investments in nutrition research more than doubled in inflation-adjusted dollars from 1985 to 2009, growing at an average annual rate of 3 percent. All of this growth is due to increased DHHS funding, especially between 1999 and 2003. In those 5 years, Congress implemented its plan to double the budget of the NIH, the lead agency within DHHS supporting nutrition research. USDA funding fell at an average annual rate of 1.4 percent between 1985 and 2009. Over the 25-year period, USDA’s share of total Federal support fell from 21 to 7 percent, and DHHS’s share rose from 79 to 93 percent.
Total expenditures are a natural way to characterize Federal support. But dollars do not reveal how many projects are supported. When charted by a count of active Federal nutrition projects, the overall Federal and agency-specific results are quite similar; however, the kink seen in the expenditures trend from the doubling of the NIH budget is not evident in the number of projects trend. This suggests that increasing project size (i.e., dollars per project) absorbed a lot of the NIH budget increase. Nevertheless, the number of federally supported nutrition research projects more than doubled from 2,178 in 1985 to 4,419 in 2009, growing at an average annual rate of 2.9 percent. From 1999 to 2009—after the NIH budget doubled—the number of DHHS-supported projects grew 7.4 percent annually while USDA-supported projects fell by 2.8 percent annually.
Research Focus Shifts to Addressing Chronic Conditions and Diseases
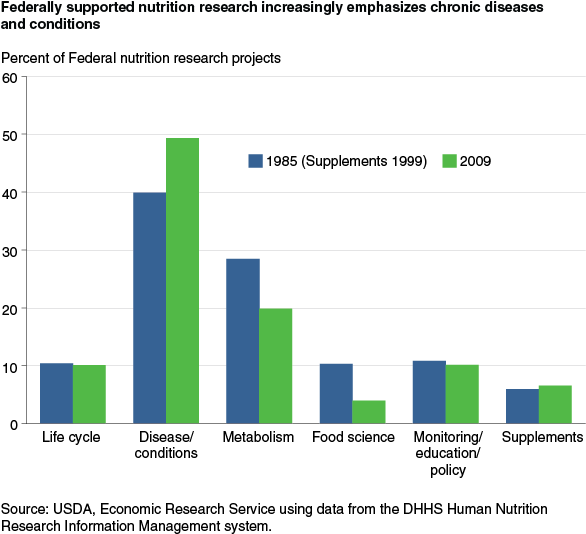
From 1985 to 2009, agency budget appropriations largely explained the aggregate trends in Federal support for human nutrition research. These aggregate trends altered the structure of Federal support by changing the funding balance among Federal agencies. To the extent that USDA and DHHS have different missions and use different research funding mechanisms, these and other influences have shifted the distribution of Federal support between nutrition research topics. For example, USDA has been the principal supporter of research on food science, the application of basic sciences and engineering to study the physical, chemical, and biochemical nature of foods and the principles of food processing. Food scientists might study how physical properties of food proteins might be altered by chemical modification. That area of research declined along with USDA’s share of Federal nutrition research support.
The HNRIM data system identifies the nature of the nutrition research conducted within each project using 37 nutrition topics. The topics make it possible to precisely describe the contribution of a specific project, as most projects address multiple topics. For example, in 2004, USDA supported a project titled “obesity prevention for preschool children.” The researchers described their project as speaking to three topics: Infant/Child Nutrition, Obesity/Anorexia/Appetite Control, and Other Research in Nutrition Education.
To sort out the broad changes in nutrition research areas receiving Federal support, ERS researchers grouped the 37 topics into 6 major research areas, weighting the projects by their share in each of the 37 topic areas.
| Research area | Description |
|---|---|
| Nutritional Requirements Throughout the Life Cycle | Studies of normal human nutritional needs for people in different stages of life |
| Disease, Injury, and Conditions | Studies of nutrition and prevention, amelioration, or treatment of diseases, injuries, infections, and conditions |
| Metabolism and Metabolic Mechanisms | Studies of nutrient variables and nutrient mechanisms and metabolism |
| Food Science | Studies of nutrition and food science |
| Nutrition Monitoring, Education, and Policy | Studies of dietary practices and behaviors of human populations |
| Dietary Supplements (added in 1999) | Studies of the composition and function of dietary supplements in human nutrition |
Over the 1985 to 2009 period, Disease, Injury, and Conditions and Metabolism and Metabolic Mechanisms remained the two largest research areas. In 2009, they together constituted 69 percent of total Federal portfolio of projects, little changed from 1985. However, as support for research in obesity, heart disease, cancer, and diabetes grew, the Disease, Injury, and Conditions area grew in portfolio share from 40 percent in 1985 to 49 percent in 2009, while the Metabolism and Metabolic Mechanisms area dropped from 28 to 20 percent.
The other research area that experienced a significant change in Federal support is Food Science, a topic largely supported by USDA. The Federal share of active projects in this area declined from 10 to 4 percent. Comparing portfolio shares tells us how the allocation of support changed over time, but does not account for the overall level of Federal support. In 2009, the Federal Government supported over twice as many active projects as in 1985. For the Metabolism and Metabolic Mechanisms research area, the number of projects supported increased even though the share in the portfolio declined. For Food Science, both the number of projects and portfolio share declined. These changes also reflect trade-offs between support for research on nutritional deficiencies and support for research on chronic conditions and diseases.
More Research Being Funded Through Competitive Grants
Over the 1985-2009 period, the organizations that perform nutrition research changed. More research is funded through competitive grants to non-Federal researchers than through Federal nutrition laboratories or land-grant universities. (A land-grant university is an institution of higher education in the United States designated by a State to receive the benefits of the Morrill Acts of 1862 and 1890. The Morrill Acts funded education institutions by granting federally controlled land to the States.) The share of Federal nutrition research projects performed by government researchers fell from 12 percent in 1985 to 6 percent in 2009. Land-grant universities are also performing a smaller share of federally supported nutrition projects—dropping from 34 percent in 1985 to 22 percent in 2009.
The share of federally supported nutrition research performed by non-land-grant universities, private companies, and other institutions (medical schools, hospitals, and research institutes) increased over the 25-year period. Non-land-grant universities and colleges increased to 41 percent of total nutrition projects in 2009, while other institutions increased their share of all active federally supported nutrition projects from 22 to 29 percent. Private companies performed just 1 to 2 percent of projects in both 1985 and 2009.
At this time, likely impacts of these changes in funding sources on research productivity are unknown; research productivity itself is an active research area, and the important questions have not yet been answered. Questions remain regarding how the type of funding influences the selection of topics studied, the innovation of the research and/or its commercial orientation, and the discovery and dissemination of knowledge. Competitive funding allows all researchers to have their ideas heard, and thus offers a strong possibility that research with the greatest chance of success and greatest impacts will be funded first. On the other hand, more stable, longer term funding to Federal nutrition laboratories or land-grant universities might emphasize long-term outcomes with a high tolerance for initial failure, and allow creativity and flexibility to pursue unanticipated lines of inquiry as research unfolds. So far, none of the conventional funding distinctions—research conducted by scientists employed by the Federal Government versus research conducted outside Federal agencies, competitive grants versus funding targeted for specific institutions—has been proven to be superior.
The United States has a diverse and multidisciplinary nutrition research system with numerous sponsoring organizations and thousands of active researchers. The body of knowledge this system produces serves as the foundation for progress toward better health. However, maintaining this foundation is not guaranteed; it depends on the resources provided by sponsoring organizations and on how research topics are selected and funded. Understanding the structure and function of the U.S. nutrition research system can help identify current and emerging issues and the research gaps or opportunities requiring further scientific inquiry.
This article is drawn from:
- Toole, A.A. & Kuchler, F. (2015). Improving Health Through Nutrition Research: An Overview of the U.S. Nutrition Research System. U.S. Department of Agriculture, Economic Research Service. ERR-182.